 |

|  | What is Intrathecal Drug Delivery ?
|
Principles of drug
delivery
Many studies have demonstrated the efficacy of opioids, such as morphine,
in the management
of pain. Pain-relieving drugs can be delivered via several routes of administration,
including:
- Systemic delivery - typically given first line
- Intraspinal (epidural and intrathecal) delivery
- given when patients experience intolerable side effects on systemic
drugs
|
|
Pain-relieving drugs can be delivered orally, rectally,
transdermally or given as an injection (intravenous, subcutaneous, intramuscular).
These forms are called systemic delivery because the pain-relieving drug
circulates throughout the patient's entire body
|
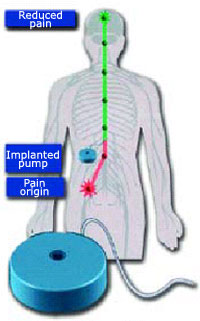
Implanted intrathecal drug
delivery system |
Pain-relieving drugs can
also be delivered intraspinally. Intraspinal delivery can be given in one
of two ways;
into the epidural space or into the intrathecal space. Pain-relieving drugs
delivered epidurally also circulate systemically. By contrast, pain-relieving
drugs delivered intrathecally circulate only in the cerebropsinal fluid
(CSF). |
Challenges of delivery of pain-relieving
drugs
Several challenges accompany delivery of pain-
relieving drugs, including: |
- Barriers to the site of action
- Dosing issues
- Potential adverse events
|
|
Barriers to the site of action
One challenge with delivery of pain-relieving drugs is that these drugs
are water-soluble.
A collection of anatomical structures exist that slow or prevent water-soluble
molecules from entering the brain and nervous system. This natural barrier
is called the blood-brain barrier. Systemically delivered pain relieving
drugs must cross the blood-brain barrier to reach the site
of action (e.g. morphine must reach the opioid receptors in the dorsal
horn). However, because
of their water solubility, these systemically circulating molecules cannot
easily pass through the blood-brain barrier. As a result, larger doses
of the pain-relieving drugs may be required for efficacy.
Intraspinal pain-relieving drugs (e.g. epidural
and Intrathecal morphine) are delivered directly
to the site of pain transmission (thereby bypassing the blood-brain barrier).
However, while both epidural and Intrathecal routes transport drugs via
CSF circulation, epidurally administered pain-relieving drugs must first
cross the dura (the protective outer layer of the spinal cord) before
entering the CSF. Therefore, when the epidural route of delivery is used,
more time and higher doses are required for the pain-relieving drugs to
reach their appropriate receptors in the dorsal horn compared with delivery.
Dosing issues
Dosing issues are of special concern in the systemic delivery of pain-relieving
drugs as a result
of the adverse effects associated with these compounds. For example, large
doses of systemic opioids may be required to treat severe pain. The larger
the dose requirement, the more adverse effects a patient is likely to
experience. Therefore, a reduction in pain may be achieved at the cost
of such adverse effects as a reduction in a patient's alertness and mobility,
nausea, vomiting, constipation, dizziness and dysphoria.
Due to the substantially lower dose required, intraspinal
delivery may offer effective pain relief
with fewer potential adverse effects for patients with chronic intractable
pain who are experiencing inadequate pain relief or intolerable side effects
on high-dose systemic pain-relieving drugs.
In many cases, the Intrathecal pain-relieving drug dose may be reduced
to 1/300th of the oral morphine dose.
|
|
Oral
to intravenous -3:1
|
|
Intravenous
to epidural - 10:1
|
|
Epidural
to intrathecal - 10:1
|
|
Oral
to intrathecal - 300:1
|
|
Typical
dose conversions for pain-relieving drug delivery
|
Potential adverse effects of morphine
Regardless of the route of delivery, pain-relieving drugs can cause adverse
effects. However,
most adverse effects can be effectively managed by reducing the amount of
drug circulating systemically in the patient's body. As IDD requires a lower
dose of pain-relieving drugs than systemic drug delivery, IDD can minimise
many of the potential adverse effects of pain-relieving drugs or decrease
their severity. |
| Criteria |
Systemic
delivery |
Epidural
delivery |
Intrathecal
delivery |
| Method of delivery |
.
Must cross the blood-brain barrier before reaching the site of action |
. Must cross the dura before reaching the
site of action
|
.
Directly infused into the CSF; bypasses the blood-brain barrier |
| Potential adverse events |
. More potential for adverse events than intraspinal
delivery including constipation lightheadedness, dizziness, sedation nausea
and vomiting
|
. Greater potential for adverse effects than
intrathecal delivery
|
. Lowest potential for adverse effects
. Potential adverse effects such as pruntis
and urinary retention can usually be effectively managed under a physician's
care
|
| Dosage requirement |
. Substantially higher dosage required than
intraspinal delivery
|
. Higher dosage required than intrathecal,
but lower dosage than systemic delivery
|
. Lower dosage required
(1/10th epidural, 1/300th oral)
|
| Comparison of delivery routes |
Intrathecal drug delivery systems
Intrathecal drug delivery (IDD) delivers small doses of pain-relieving drugs,
such as morphine,
via a pump (SynchroMed II/SynchroMed EL/Isomed) that is placed surgically
under the skin,
directly into the CSF. This route of administration offers the potential
for more potent analgesia
with fewer side effects than systemic routes of administration. Studies
have shown that patients treated with intrathecal pain-relieving drugs did
not experience many of the undesirable side effects observed with oral/parenteral
narcotics. This is due to the fact that intrathecal drug infusion is directed
to the spinal cord (the site of action), meaning that smaller doses are
required than with oral or intravenous methods. |
Intrathecal
drug delivery system components
An IDD system consists of two basic components that are placed in the body
during a surgical procedure: |
|
|
|

|

|
SynchroMed EL
Intrathecal
(available
with a 10mL or 18mL)
|
SynchroMed
II Intrathecal
drug delivery system
(available with a 20mL or 40mL)
|
|
Pump
The pump is a round metal device that stores and automatically releases
prescribed amounts of pain medication through the catheter directly into
the intrathecal space. The exact dosage,
rate and timing prescribed are entered in the pump using a programmer,
an external computer-like device that controls
the pump's memory.
As the pump has a predetremined flow rate, the daily dosage
has to be calculated before the pump is filled with medication. Information
about the prescription is stored in the pump's memory.
|

Isomed drug delivery system |
|
The pump holds a finite amount of medication, which
means it needs to be refilled periodically.
This is performed by inserting a needle through the skin and into the
pump's reservoir.
Refill intervals are typically every 1-3 months, although this may vary
depending on individual prescriptions.Medtronic also have a constant rate
pump called Isomed which is mainly used
for chemotherapy.
|
|
Catheter
The catheter is a small soft tube. The catheter passer is used to help
put the catheter in.
One end of the catheter is connected to the pump and the other is placed
into the area
surrounding the spinal cord (intrathecal space).
|
 Fully
functioning Intrathecal drug delivery system
Fully
functioning Intrathecal drug delivery system
|
Functioning intrathecal drug delivery system
The functioning IDD system sends small, programmed
amounts of pain-relieving drugs from the pump, through
the catheter directly into the CSF in the intrathecal space,
where there is a high concentration of receptors.
Benefits of Intrathecal
Drug Delivery
Clinical efficacy of IDD
- Clinical studies have shown that IDD can provide:
- good to excellent pain relief in 65-80% of selected
patients, and improvements in activities of daily living.
[1,2,3]
- a reduction in side effects observed with oral/parenteral narcotics
e.g. tolerance and addiction. [4,5,6]
|
|
- less sedation and
constipation than systemic drugs. [7]
- lower doses than those required with oral and intravenous methods e.g.
the equivalent of 1/300th of an oral dosage of morphine can
often provide effective pain relief. [8]
- Patients who are
required to change from oral to intrathecal drug administration experience
an improvement in long-term pain relief.
Intrathecal drug delivery in CRPS
- In a randomized, double-blind study [9], bolus
intrathecal injections of baclofen and continuous intrathecal baclofen
were given to 7 women with CRPS type I and II:
- 86% of patients receiving bolus intrathecal baclofen achieved complete
or partial
resolution of dystonia of the hands.
- 50% of patients receiving continuous baclofen regained normal hand
function, and 33% also regained their ability of walk.
- In a prospective study in 15 patients with chronic
intractable pain who received intraspinal morphine [10], 11 patients
experienced 'good to excellent' pain relief, and 6 patients were able
to return to work.
|
References
1. Winkelmuller M et al. Journal of Neurosurgery 1996;85:458-67
2. Penn R, Paice J. J Neurosurg 1987;67:182-6
3. Paice J et al. J Pain Symptom Manage 1996;11:71-80
4. Follett K et al. Pain 1992;49:21-25
5. Gilmer-Hill H et al. Surg Neurol 1999; 51:6-11
6. Portenoy RK and Savage SR. J Pain Symptom Manage 1997;14(suppl. 3):S27-35
7. Gianino. Practical Pain Management 1996:127-154
8. Krames ES. J Pain Symptom Manage 1996;11:333-352
9. Van Hilten BJ et al. N Engl J Med 2000;343:625-30
10. Kanoff RB. J Am Osteopath Assoc 1994;94:487-93
|


